By Riley Kaminer
One day seven years ago, Steven Charlap got a call from his brother, a practicing cardiologist. “He told me he had been diagnosed with two cancers a week apart,” Charlap told Refresh Miami. Within the year, his brother passed away.
This experience shook Charlap, a doctor himself: “Suddenly I said, ‘Wait a second, maybe I don’t know as much about genomics and lifestyle and the ultimate impact it has on human health.’”
“Why did doctors not catch my brother’s cancer earlier given our extensive family history of early cancer on my father’s side that resulted in at least five relatives dying before the age of 61?” Charlap asked himself at the time.

Charlap, who after having studied to be a surgeon completed an MBA at Harvard and started two businesses, would spend years studying to determine the answer to this question: our system for primary care is broken, specifically when it comes to diagnosing what is wrong with patients.
“Doctors don’t spend enough time with patients,” said Charlap, positing that these family doctors are paid insufficiently – at levels lower than the 1970s, when adjusted for inflation. “They’re not paid to prevent early or to detect diseases. They’re paid to treat symptoms.”
These doctors also suffer from cognitive bias, explained Charlap. “If five people walk in with symptoms that look like COVID, why wouldn’t I think the sixth patient has COVID? When in fact, they have leukemia.”
What’s more, when a patient leaves the doctor’s office, there is rarely any follow up. All of this translates to as many as 45 million diagnostic errors being made each year in the US. Diagnostic errors lead to 250,000 lost lives and nearly a trillion dollars every year.
But the blame does not wholly sit with the doctors themselves. Through his research, Charlap has learned that more than 50% of Americans have lied to doctors about things that might embarrass them, while 30% of people with mental health conditions do not disclose them to medical personnel.
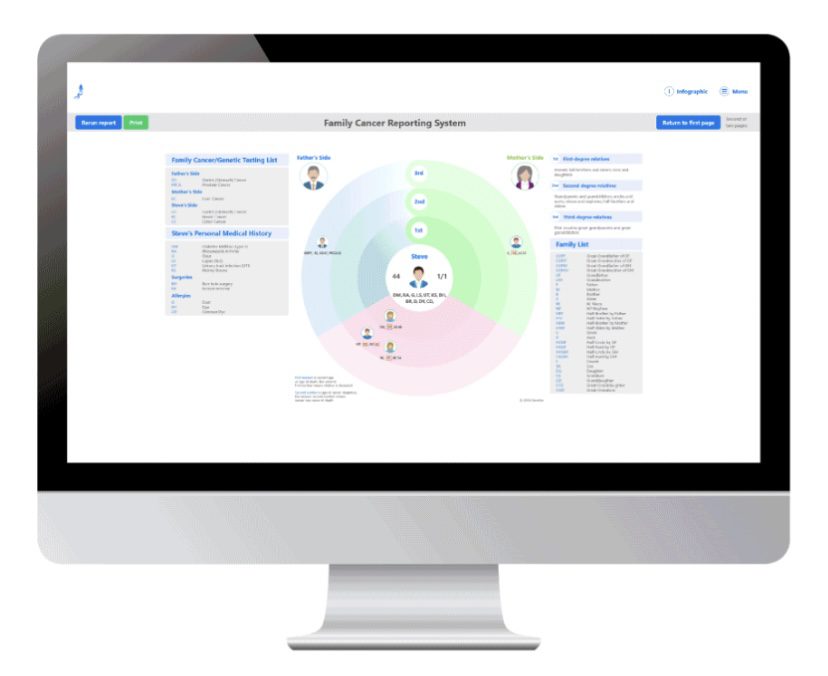
It is in this context that Charlap decided in 2019 to start developing a digital tool to overcome some of these hurdles. He founded SOAP Health and developed a patented and clinically validated virtual medical assistant. This digital tool is a conversational AI-powered animated character that interviews patients and does a risk assessment.
According to Charlap, an early pilot test showed that in 100% of cases, the digital system identified information a doctor missed. In two out of three cases, it caught something important that was missed by the doctor, such as a risk for diabetes or a cancerous syndrome. Another study showed that the system reduced the amount of time it took for a doctor to undertake and document an intake by 66% thanks to its comprehensive risk assessment tool and ability to automatically create ‘smart’ notes on the doctor’s behalf.
Charlap hopes that SOAP will help doctors reduce their burnout. “We’ve got to make operating as a doctor more like an air traffic controller. controlling multiple planes coming in, where life and death is equal to the care of an individual patient.”
Since launching, SOAP has raised over $3 million in seed funding. The Boca Raton-based company has two of its 17 full-time employees in South Florida, with another coming here soon. And South Florida will likely play a major role in the company’s growth, since it is in pilot discussions with a variety of local hospitals and care providers. On top of having taken part in the FAU Tech Runway and Endeavor’s accelerator, the startup has also participated in an accelerator from the Mayo Clinic and MassChallenge.
Ultimately, Charlap’s goal is to improve early disease detection and prevention. “We can do that by creating precision patient profiles,” he said, since most electronic health records are at the very least incomplete – and at worst inaccurate.
READ MORE IN REFRESH MIAMI:
- What happened in Miami tech in 2022? We’ve got the recap for you!
- This smart label for medications can improve healthcare outcomes at scale
- Boca-born Reachlink makes behavioral health services available to all
- Miami-based Index Health secures $6M seed round
- Assure Health raises $8.7M seed round to expand virtual healthcare platform
- Ostro lands $45M to ‘bring e-commerce software to healthcare’
- The hottest technology in Miami? Exowatt raises $20M, launches renewable energy solution - April 22, 2024
- This Earth Day, let’s shine a spotlight onSouth Florida innovators building a greener world - April 22, 2024
- Dataplor’s $10.6M Series A will help usher in the next generation of global location intelligence - April 22, 2024





